Advertisement
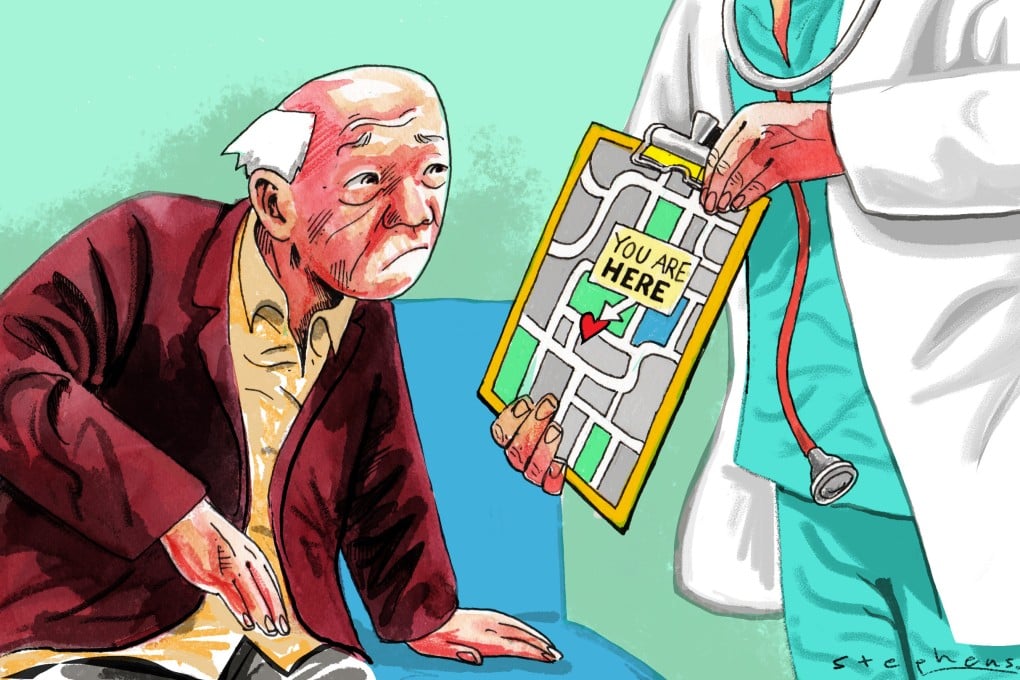
Opinion | For Hong Kong’s healthcare reforms to work, better policies are needed for its ageing population
- Latest reforms reflect an ageing policy still too narrowly focused on disease prevention rather than ageing successfully
- Affordability of chronic disease management must be tackled as well as health literacy and the wider socio-economic factors that support good health outcomes
Reading Time:3 minutes
Why you can trust SCMP
1
Hong Kong’s public hospital emergency rooms are typically swamped during the winter flu season. The recent jump in Covid-19 cases is aggravating the egregious situation. It is not uncommon to see waiting times exceeding eight hours – an outright ordeal for patients who rely on public healthcare.
The situation partly reflects the underdevelopment of Hong Kong’s primary care system. Around 60 per cent of accident and emergency cases are semi-urgent or even non-urgent, and most could be handled by community doctors. It is perhaps opportune that the government has announced the Primary Healthcare Blueprint, given the challenges of the city’s ageing population.
Hong Kong’s healthcare system is among the most efficient in the world, but it clearly shows signs of overload and a lack of sustainability. The government blueprint has rightly emphasised a paradigm shift for the treatment-oriented system to become one more focused on prevention, with district health centres taking on screening, education and chronic disease management in the community.
Advertisement
Patients are also encouraged to have a regular family doctor as their first contact point for healthcare and the management of chronic conditions. A Hong Kong study found that patients with multiple ailments who had a regular source of primary care were 23 per cent less likely to be hospitalised than those who did not.
But, for all the efforts to improve primary care in Hong Kong, structural barriers have not been considered sufficiently. Affordability of chronic disease management has long been an issue. Older people are among the most frequent users of the public system – three-quarters of elderly Hongkongers have at least one chronic condition, which usually requires multiple follow-ups, long-term medication and investigations.
Advertisement
Whether the financial incentives under the chronic disease co-care scheme in the blueprint are adequate for older patients to pursue disease management in the private sector remains to be assessed.
Advertisement
Select Voice
Select Speed
1.00x
.jpg?itok=x0VyVnpg&v=1655360011)